BLOG
A Tool for Dizziness Diagnosis
THE WHY? Empower PTs to make the ED experience better for people with invisible acute crises. People need support when they are in crisis and are often dismissed as having a mental health issue with a psych consult in the ED due to poor coping skills and self regulation.

Spilling Out of the Box – A Word for Students
You’re not a one thing. Don’t settle. Keep building you and break out of the box.

The First Annual Top of Scope Summit
The format of the course will be 15 minute presentations followed by live interactive discussion with the presenters and your colleagues. Each presentation will be drilled down to the essentials so you get short presentations with maximal impact. Perfect for the expansion of the ED PT toolkit.

Embracing the Future
“When people think that our services are only valuable in the CMS slide show scale of reimbursement for eight-minute CPT codes, that’s a failure on your part to understand the value of what you do as a clinician and what you provide.”

Why ChatGPT Doesn’t Like ED PT
I spend so much of my time explaining why PTs are critical in the ED. We’re often the right provider at the right time. PTs in the ED have been shown to save costs, improve patient and provider satisfaction, expedite operations, and even decrease opioid use. So, why wouldn’t you want a PT in the ED?
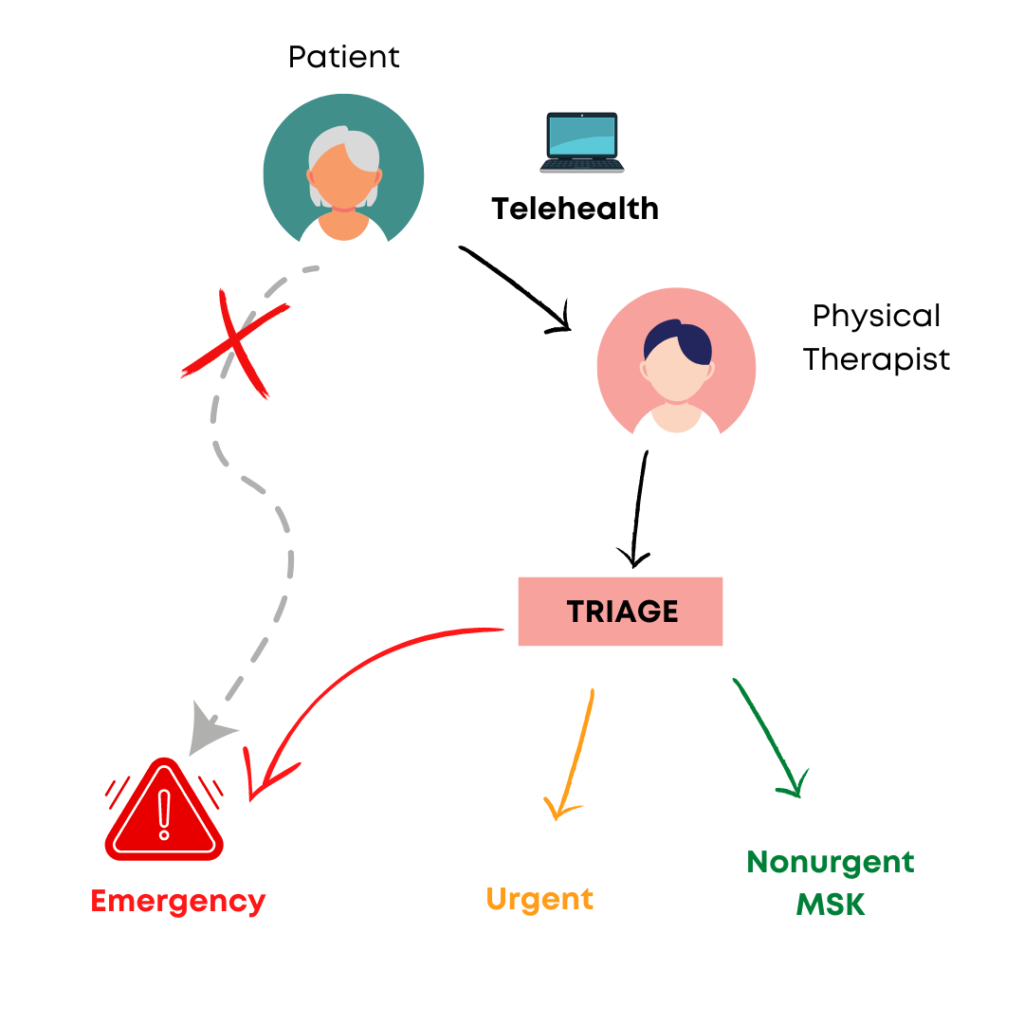
How Physical Therapists Outside the Emergency Setting Could Help Save It
Digital physical therapist triage has the potential to decrease unnecessary ED visits, thereby reducing costs, improving health, and raising patient satisfaction.

Staying on the Softer Side
This is when it really hit me. That reminder of the tragedies of life. Most of the patients I was planning to see were my age or younger, beset by, at best, completely life altering circumstances laden with permanent disability, and at worst, fatal diagnosis. That heaviness might not impact others the way it does me. But for me it feels like this huge weighted blanket of grief mixed with possibility. I remembered why I prefer the acute emergency, the limited involvement, the hopeful possibilities in the ED, and why I had somewhat distanced myself from this type of patient care.

Take 5 – IFOMPT Cervical Framework
A 70 year old male comes into the ED with episodic neck pain and headache. He has a history of hypertension, CVA, and headaches that feel similar to this one. In the past, PT treated his neck pain. You are seeing him in the ED as their first point provider. What do you do? How do you know that this is truly musculoskeletal pain versus something more sinister?
Migraine in the ED
By recognizing the unique challenges faced by migraine patients in the emergency department, physical therapists can play a vital role in providing comprehensive care, improving patient outcomes, and minimizing the impact of migraine on their lives. Together, we can create a more supportive and understanding healthcare environment for those living with migraine.
Take 5 – Canadian C-Spine Rule
A 33 year old patient comes into the ED after getting rear-ended during rush hour traffic on Friday afternoon. They were in stand still traffic when they were caught off guard and hit from behind by a car going 10 mph. The patient ambulated into the ED with family present and stated that they felt fine until an hour ago when they started to get a headache. What should you do for this patient? Do they need imaging? What needs to be ruled out before you can treat them for whiplash and/or concussion? How much time do you need? What resources are required?

ED PT Red Flag Questions – In Spanish
My name is Alejandro, I help healthcare professionals in physical therapy confidently serve their patients that speak Spanish. My mission is to help others provide better quality of care by improving communication and understanding by teaching Spanish specific to Physical Therapy in any way that saves time, is applicable, and is enjoyable.
You’re the Dizziness Detective in the ED
A 52 year old patient sits very still in a chair at your facility’s Emergency Department, with her eyes closed and an emesis pan in arm’s reach. One glance at the chart tells you what you’ve already guessed – the patient came in with complaints of acute vertigo, the nurse recently gave her Zofran to manage nausea, and an MRI of her head has come back negative for stroke. Of course, you know that an MRI can be falsely negative for stroke in at least 12% of patients in the first 24-48 hours from symptom onset (Kattah et al., 2009). As the physical therapist assigned to the ED and renowned “dizziness detective,” you’ve been asked to help out. What do you do first?

Take 5 – The Ottawa Knee Rules
A patient comes into the ED after twisting their knee falling off their skateboard. They are having a hard time walking and want to make sure their knee is okay so they can go to school and play soccer on their varsity high school team. What do you need to rule out? How do you know if you need imaging? And how long will all of this take? Based on the injury, how will this affect your plan of care and management of this patient?
The Million Dollar Question
We are often asked by therapists or managers: How can we demonstrate the financial benefit of having Physical Therapy in the Emergency Department? Unfortunately, it’s complicated.

Take 5 – Social Determinants of Health: Are You Measuring Them?
Social Determinants of Health (SDH) may be more influential over health outcomes for musculoskeletal (MSK) conditions compared to direct medical treatment.
Take 5 – Let’s Look at Diagnostic Accuracy of the Ottawa Ankle Rule
Gomes YE, Chau M, Banwell HA, Causby RS. Diagnostic accuracy of the Ottawa ankle rule to exclude fractures in acute ankle injuries in adults: a systematic review and meta-analysis. BMC
Take 5 – Direct Access Physiotherapy to Help Manage Patients With Musculoskeletal Disorders in an Emergency Department: Results of a randomized controlled trial
A patient comes into the ED with back pain from an injury at home when they went to pick up a heavy box. Their pain hasn’t improved since the incident yesterday and they want to get evaluated for an injury and pain control. Which provider(s) can help them? And how can they be helped? How can we ensure the patient gets better today, one month, and three months from now?
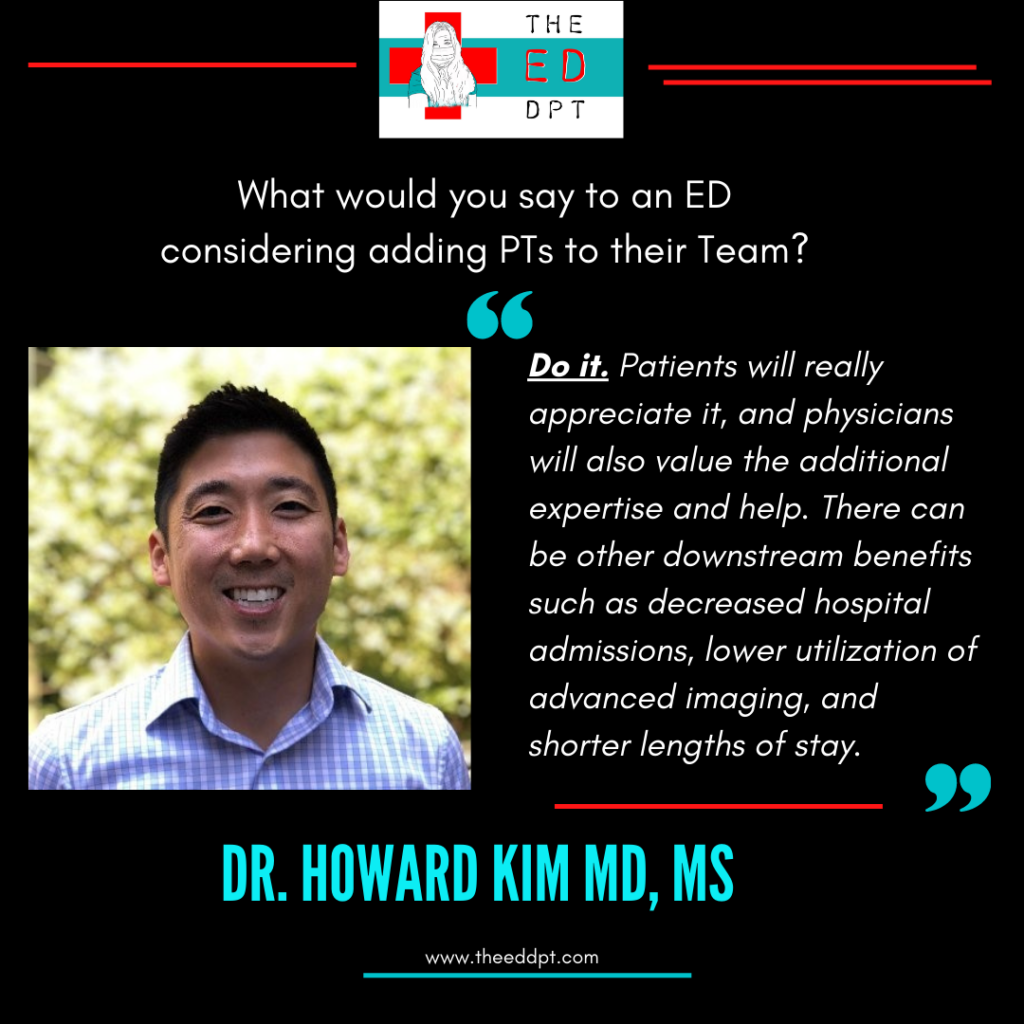
Researching a Path to Better Care Through ED PT
I think just understanding that the ED team really wants to hear your opinion on the diagnosis and recommendations for care is a great place to start. As I alluded to before, we generally have a laid-back culture and flat hierarchy and will readily acknowledge that you have unique expertise in whatever clinical area we’ve asked for your help in. The ED environment is always really busy and we’re doing a thousand things at once, so we’ll always look like our hair is on fire – but just knowing that we see you as value added is a great mindset to come from. In terms of actual communication strategies, I would say keep it short and simple? We tend to be more interested in the punchline than the plot development/background. And then if there’s disagreement, just standard communication principles: try to understand where both parties are coming from and keep things focused on the patient.
Take 5 – H.I.N.T.S. to Diagnose Stroke in Acute Vestibular Syndrome
You’re asked to see a patient in the ED presenting with vertigo. They are constantly dizzy, unsteady with gait, nauseous and vomiting, and reporting that their symptoms started yesterday and worsened over the course of an hour. How do you know what type of vertigo they have? And how can you rule in/out central or peripheral causes for vertigo? Has any imaging been done? Does that even matter?

Strictly Speaking, Physical Therapists Belong in the Emergency Department
I had to demonstrate my ability to help the team through constant communication and education of our role as a therapist.
Take 5 – Vestibular Physical Therapy in the ED
I know some PTs shy away from the opportunity to develop their skill set in vestibular PT. However, with appropriate training and continuing education and use of vestibular clinical pathways, PT practice in the ED can improve patient outcomes and hospital processes for the better.
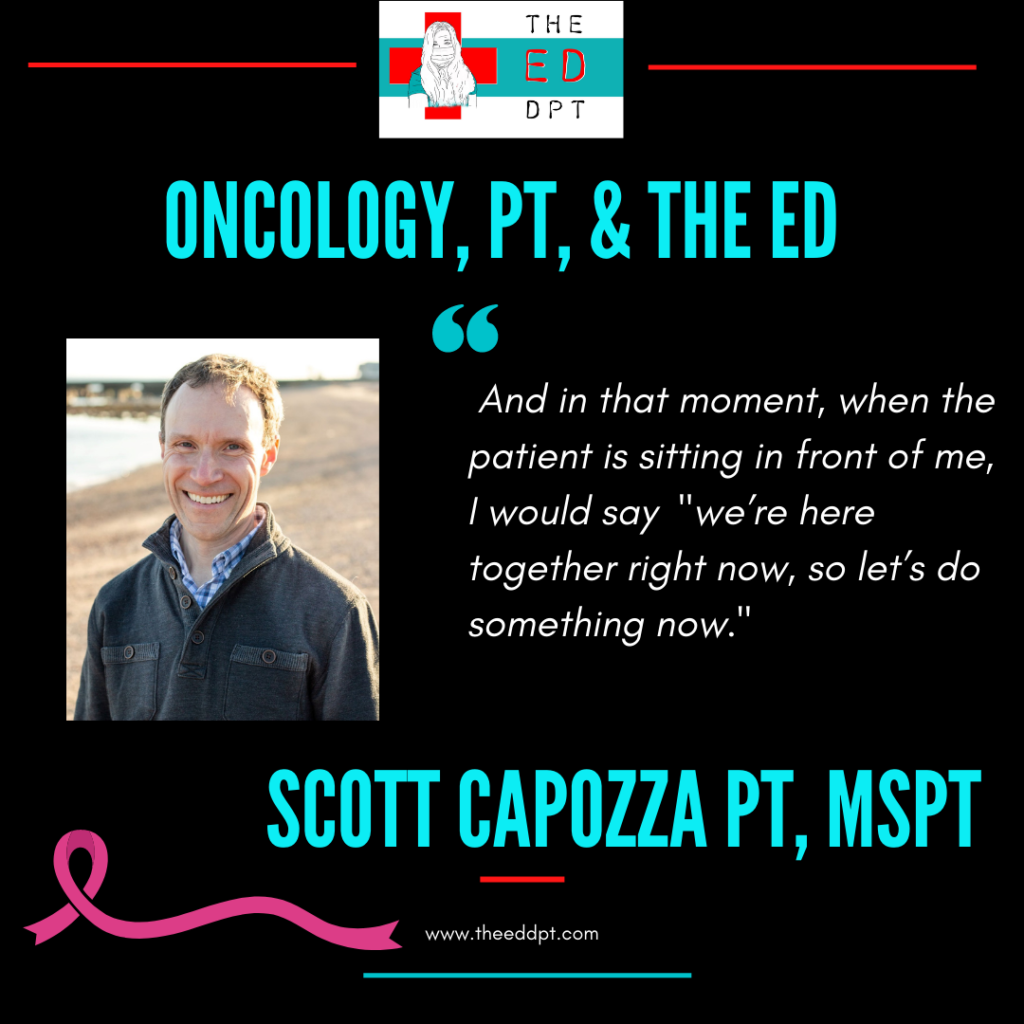
Oncology & PT Considerations for the Emergency Department
A cancer diagnosis comes with a multitude of emotions, including the loss of control. A person who is newly diagnosed with cancer may not feel that they have any control over their lives, as they now have multiple appointments to attend. We as PTs can offer people living with cancer some sense of control; we can educate on safe mobility, validate their concerns, and provide a consistent calm through the storm that is a cancer diagnosis.
Physiotherapy in the Emergency Department in Australia
Describe how you became involved in Emergency Department Physical Therapist Practice. I have a broad range of experience across inpatients and outpatient hospital services, with a focus on orthopaedics (elective

How to Build a Thriving Emergency Department Physical Therapist Practice
This 2-day, in-person course will prepare you to create a thriving Emergency Department Physical Therapist practice whether you are working from the ground up or enhancing your current program.
Take 5 – October
No time for reviewing the literature? No problem.
Dr. Jacobsen summarizes pertinent literature to save you time & improve your practice.
Researching Emergency Physical Therapist Practice
I first became interested while lying in the ED after being hit by a car…
I’m Seen For What I am – A Doctor of Physical Therapy
The emergency department is a unique unit because it requires the clinician to utilize everything they have learned throughout physical therapy school and previous clinical experience.
From Rural Private Practice to the Emergency Department
I showed up day one with nothing, just me. No equipment, no tools except my hands and my brain.
Making it Mindful
“Mindfulness can be a lifestyle. It is a non-judgemental existence assessing what is going on with you and around. With mindfulness you decide how you want to respond, it can start with an intentional breath to check in with yourself.”
Veteran’s Affairs, the ED, & the PT
One must be adaptable, flexible, bold, and efficient in their encounters with patients and providers alike. Particularly in the veteran population, a little warmth and choice words go a long way to quickly build a therapeutic alliance.
From the Bedside to the QI Side
Dr. Ryer is the Senior Project Coordinator in Senior Services at Advocate Aurora Health, located in Wisconsin and Illinois. She is a Doctor of Physical Therapy who is board certified

Bridging the GAP
I designed an intervention called GAPcare (the Geriatric Acute and Post-acute fall prevention intervention). The idea of GAPcare came to me after talking to our case managers. They said we really need PT in the ED to help with our patients.

The Emergency Department is No Place for Older Adults – Let’s Change That
An article by Dr. Pauline Chen sums this up nicely with her quote, “An older nurse finally pulled me aside. ‘Just admit him,’ she whispered, ‘It’ll cost more, but it’s
ED PA + ED PT = Teamwork
AMAZING. At this point I don’t know if I could go back to having to manage patients without my PT colleagues. They really help round out the care provided to patients in the ER.

The Innovator
I started to see not only the value in this practice but also the potential.

The Legend
Meet Lisa TenBarge PT, DPT. Dr. TenBarge has been practicing in Emergency Department Physical Therapy in Flagstaff AZ since 2004 and has presented on the subject dozens of times on
From Outpatient to All Patient
Personally, my biggest adjustment was a change in mindset. In outpatient, my focus was improving patient’ pain experiences immediately to build a relationship moving forward. In the ED, my focus is to improve patients’ pain experiences to give them a path forward and guide them to outpatient. I’m making sure they are safe to return home, but not necessarily improving their pain experience to a 0, like I would shoot for in outpatient.
Home (Health) is Where the Heart Is
Advanced practice is really just all about doing the basics really well and being able to apply the basics to a much broader presentation. Students need to learn the basics really well, so they can apply them in advanced ways. That’s what I try to ensure happens.

Call On Me
I refer to myself as an acute care generalist with an emphasis on Emergency PT and ICU PT. Really, I’m a “jack of all PT trades” which has been beneficial in the ED so that I have been able to manage a wide variety of conditions.

Be a Super Model
No two Emergency Department Physical Therapy (ED PT) programs are the same. However, the most common models are the embedded model, or the on-call model. This post will help delineate the pros/cons of both so you can decide what works best for your program. I’ll let you decide, which one is the “Super Model.”

What to do in a Disaster
“We do so much more than we are recognized for doing that it is important to practice up to our education and potential.”

One Man Show
What is your philosophy about what makes an ideal ED PT?
Meet people where they are and do what you can for them. You can’t save or help everyone but you can always listen and provide comfort.

What is the Flow?
Question – What are you allowed to do in the ED? Generally how does the process of seeing a patient go?
The short answer? As every physical therapist must, it depends.

Feature Friday – Meet Dr. Bush
“Personally, as a new grad, this setting can be very intimidating. I really had to learn to trust my knowledge as a PT and speak up for my patients and myself when I believe their plan of care needs to be something different than what the doctor originally suggests.”

Back to Back to Back
Imagine you are at work, you’ve just grabbed a 50 pound box to carry, but as you come up, you feel a pop in your back. Immediately you’re on your knees, overcome with pain…

Feature Friday!
When I first started working at my current hospital, there was no structured therapy program in the ED, but we would be called down for select cases to support, as needed. Our PTs established a substantial therapy program and we were consulted much more frequently at that point. I volunteered to be part of the small team of OTs that would float down to the ED, where I worked with our PTs to advocate for OT involvement and appropriate consults. I was a relatively new grad and really loved that I felt like I could practice at the top of my scope. When the opportunity arose last summer to spend some time full time in the ED, I jumped on it.

Welcome to all Things Emergency Department PT!
Rebekah Griffith PT, DPT – The ED DPT Let’s begin at the beginning! Hi! I’m Dr. Rebekah Griffith, the Emergency Department (ED) Physical Therapist behind The ED DPT. The ED
"A physical therapist in the ED is part of a multidisciplinary team working alongside physicians, physician assistants, nurse practitioners, occupational therapists, paramedics, EMTs, social workers, case managers, behavioral health providers, and more."

