Dr. Ryer is the Senior Project Coordinator in Senior Services at Advocate Aurora Health, located in Wisconsin and Illinois. She is a Doctor of Physical Therapy who is board certified in Geriatrics with nearly twenty years of clinical experience in a variety of clinical settings. Her focus is on interdisciplinary geriatric care with emphasis on fall prevention and expanding and improving quality of Geriatric ED throughout the health system.
Dr. Ryer has created interdisciplinary fall prevention and mobility programs for the health system to improve clinical outcomes and combat hospital-associated disability and readmission. She is the co-chair of the Milwaukee County Falls Prevention Coalition and has created partnerships with a variety of community-based organizations at both the state and local level. Dr. Ryer has published multiple articles on topics related to community fall prevention and care in the geriatric emergency department as well as presenting at state and local conferences. She is active in national organizations including APTA Geriatrics and teaches locally as an adjunct professor for physical therapy in the area of geriatrics.
Describe your transition from clinical to non-clinical work.
I started my career in 2003 as an acute care therapist in a Level II trauma center and found a passion for critical care and caring for the most vulnerable populations. Over next several years experience a variety of clinical settings as well as moved into management, with positions as a lead clinician, supervisor, and director. Along the journey, I found a passion for program development and particularly for seeing a problem or unmet need in my clinical setting and seeking to change the way that things were done to do this.
My professional journey, like many was altered when I had kids and was fortunate to find my way to home health, a setting I had never considered to be a “good fit” for me. Instead, it completely solidified my passion for caring for older adults, meeting them where they were, and really seeing all the challenges and opportunities in supporting them in aging in place and in the community that had been hard to imagine when working in the hospital just trying to get them home.
Upon re-entering the hospital setting years later, the passion from home health for geriatric care brought me to seek opportunity to be involved in a new project that was considering how to provide best care for geriatric population in the emergency room. My passion in this area led me to speak up for the importance of having physical therapy and rehab services as a whole at the table in the introduction of these concepts to the health system and the creation of protocols to meet older adult needs, discharge planning, and particularly assessment of patients who had fallen.
With time, this work and my involvement led to a system level position within the geriatric emergency department implementation process as well as in leading other health-system and community efforts to improve care for older adults.
Describe some common complexities around the older adult population in the ED.
Complex medical conditions and other multiple chronic conditions that overlay making diagnosis and treatment challenging.
Environment of ED (noisy, crowded, lighting, lack of appropriate DME or beds/chairs) is not suited to older adults.
Additional care needed in selecting appropriate ED-based interventions (medications, referrals, etc) to avoid secondary complications such as confusion, delirium, fall risk.
Challenges in discharge planning and care coordination upon discharge (⅔ of older adults discharge home immediately from the emergency department.
What is a geriatric certification for an Emergency Department?
Accreditation awarded by the American College for Emergency Physicians (ACEP) that recognizes emergency departments for implementing policies and procedures, best practices, and education of staff that allows for optimal geriatric emergency care. A set of guidelines was initially developed in 2014 which serves as the framework for this accreditation, which can be awarded at 3 levels (gold, silver, bronze also known as Level I, II, and III).
Examples of Components
- Ensuring geriatric-focused education and interdisciplinary staffing.
- Providing standardized approaches to care that address common geriatric issues.
- Ensuring optimal transitions of care from the ED to other settings (inpatient, home, community-based care, rehabilitation, long-term care).
- Promoting geriatric-focused quality improvement and enhancements of the physical environment and supplies.
Examples of standardized approaches/best practices includes – 24 hour access to nutrition that meets the needs of an older adult, ensuring resources such as DME are available to be utilized in ED, and reduction/elimination of use of Foley catheters and other high risk procedures/interventions for older adults.
What would ideal state look like?
All emergency departments in U.S. would be accredited at Level III which would indicate the “basic” level of attention to improving care for older adults and acknowledging the unique needs of this population and that they are not the same as younger adults in the ED (much like all EDs have specific policies and procedures for how to address pediatrics patients presenting to the ED).
What Impacts Have you Noticed Based on Your Research?
Identified high rates of ED revisit amongst patients presenting for falls as well as amongst patients who did not receive orders for follow up care upon discharge.
Have been able to reduce ED revisits and subsequent hospital readmissions through appropriate care transitions, connection to follow up care.
Have been able to reduced ED revisits and also hospital admissions through addition resources in ED for vulnerable populations (case management involvement, social work support, physical therapy consultation).
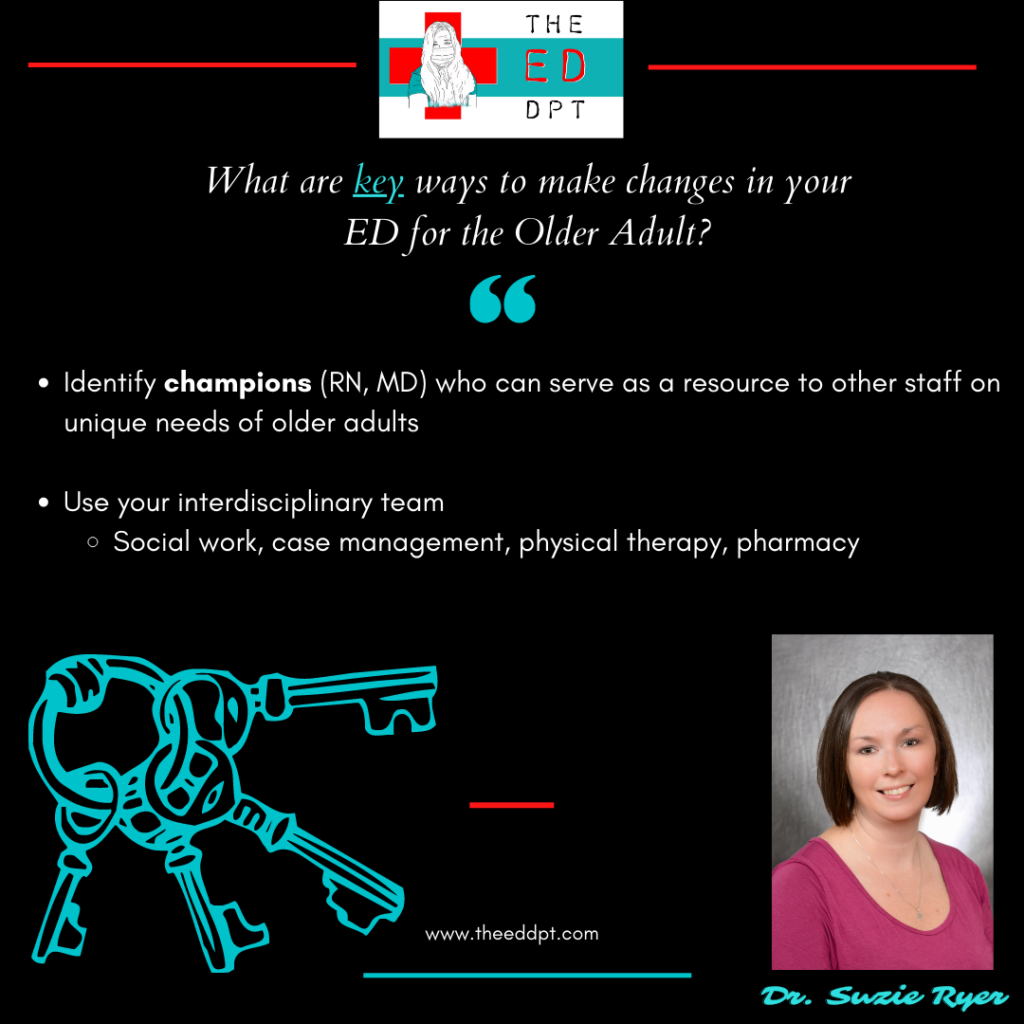
If a program isn’t ready to pursue certification, what are some key small changes you can recommend?
Work to Identify champions (RN, MD) who can serve as a resource to other staff on unique needs of older adults.
Also, make sure you have the ability to access the interdisciplinary team, specifically social work, case management, physical therapy, pharmacy to collaborate on evaluation and care transitions for older adults, even on an “as needed basis.”
Are there resources to help educate our multidisciplinary team?
- Geriatric Emergency Department Collaborative (GEDC) is a great source of education, best practices, and resources.. Provide regular webinars, toolkits, and recommendations for those getting started or just looking to learn more. There are also great resources available through Emergency Nurse Association (ENA). APTA Geriatrics also has great toolkits for assessment of older adults, particularly as it relates to balance and falls, that can be a great resource for improving practices and integrating PT into care of this vulnerable population.
Where can I learn more?
American College of Emergency Physicians www.acep/org/geda
Geriatric Emergency Department Collaborative: www.gedcollaborative.com
Journal of Geriatric Emergency Medicine
Also, take a listen to our interview with Dr. Goldberg on her research here.
Self-paced continuing education webinar here.
Who should I follow in this space?
Geriatric Emergency Department Collaborative: @theGEDC
ACEP Geriatric Section: @GeriatricEDNews
Don Melady: @geri_EM
Ula Hwang: @ulahwang
Liz Goldberg: @LizGoldbergMD
Christina Shenvi: @clshenvi
Maura Kennedy:@MauraKennedyMD
Thank you Dr. Ryer for all you do for our profession!