
Guest Blog by Helena Esmonde PT, DPT, NCS
A 52 year old patient sits very still in a chair at your facility’s Emergency Department, with her eyes closed and an emesis pan in arm’s reach. One glance at the chart tells you what you’ve already guessed – the patient came in with complaints of acute vertigo, the nurse recently gave her Zofran to manage nausea, and an MRI of her head has come back negative for stroke. Of course, you know that an MRI can be falsely negative for stroke in at least 12% of patients in the first 24-48 hours from symptom onset (Kattah et al., 2009). As the physical therapist assigned to the ED and renowned “dizziness detective,” you’ve been asked to help out. What do you do first?

After you kindly introduce yourself, you gather an efficient history. Past medical history includes hypertension and hypothyroidism. The patient had a sudden onset of vertigo sitting up from lying down 10 hours ago, provoked by rolling in bed and any head or body movements, lasting less than one minute but then with ongoing nausea since onset. No headache, no hearing changes, and no prior episodes of vertigo in this patient’s history.
You start with your streamlined vestibular screening – rule out the serious stuff first. You perform HINTS plus. This test can provide powerful clues, identifying a stroke (infarct) in acute vertigo cases with a sensitivity of 96.5% and a specificity of 84.4% (Newman-Toker et al., 2013).
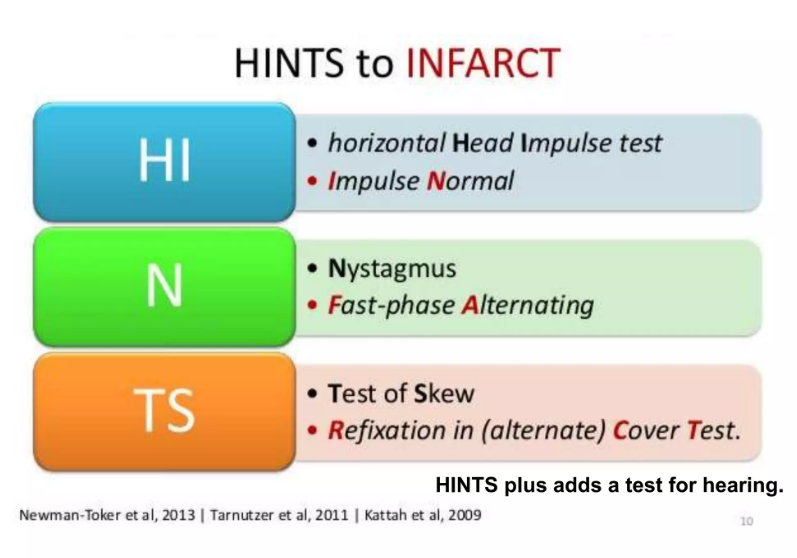
Caption: HINTS testing to rule out infarct (stroke)
Step 1: Head impulse test. No quick corrective saccadic eye movements when you move the head quickly to either side leads us away from a peripheral vestibular hypofunction. If it was positive to one side (example left), we would suspect a peripheral vestibular hypofunction (example left if head impulse test was positive to the left). Stroke is still a possibility at this point.
Step 2: Nystagmus. No spontaneous nystagmus is visible, even when the patient is wearing our infrared video goggles (here’s hoping you are able to convince your department to get some) so that we can see eye movements that wouldn’t be seen in room light. Without goggles, we just do the best we can to look for spontaneous nystagmus in room light. If there was nystagmus with gaze toward a single direction (example: right beating nystagmus) we would suspect a peripheral vestibular hypofunction (example: left hypofunction if the spontaneous beat was to the right). If there was a nystagmus that was direction changing (right beat with right gaze, left beat with left gaze, and up beat with upgaze), we could suspect a central vestibular issue such as stroke. No signs of hypofunction or stroke in this case though.
Step 3: Test of Skew. Luckily, neither eye shifts position when you cover and then uncover it. Negative skew testing points us away from a cerebellar stroke once again.
Step 4: “Plus” – hearing screening helps rule out signs of labyrinthine stroke; patient denies any new hearing loss, so we are looking good here as well.
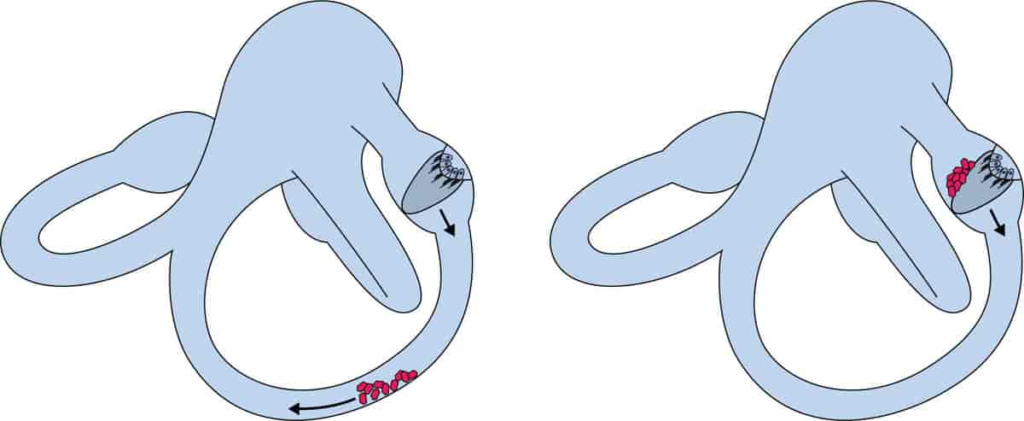
Caption: Otoconia in the posterior canal during BPPV (Creative Commons)
Now we’re ready to check for benign paroxysmal positional vertigo, or BPPV. When those tiny otoconia or crystals in our inner ear balance sensor move into a semicircular canal where they don’t belong, they can definitely cause the symptoms that our patient has been reporting. We know there’s a good chance of BPPV in this case, given the patient ‘s report of symptoms provoked by rolling in bed. BPPV is the most frequent cause of positional vertigo (Kattah, 2019). Plus, the duration of dizziness spells <1 min and dizziness provoked by rolling over in bed are independently associated with the diagnosis BPPV (van Dam et al., 2020). Clues abound here!
We start with the Dix Hallpike test, with our infrared video goggles once again in place on the patient first if we have some available. But we see no nystagmus on either side, although the patient feels pretty awful. Some clinicians would stop their assessment here, but as a seasoned dizziness detective, you know better. It’s time to test the supine roll test, which is more specific to the horizontal canal. You know it’s quite important to check for horizontal canal BPPV in the ED – in one recent study, more patients who visited the emergency room with BPPV were found to have horizontal semicircular canal BPPV than posterior semicircular canal BPPV (Kim et al., 2023).
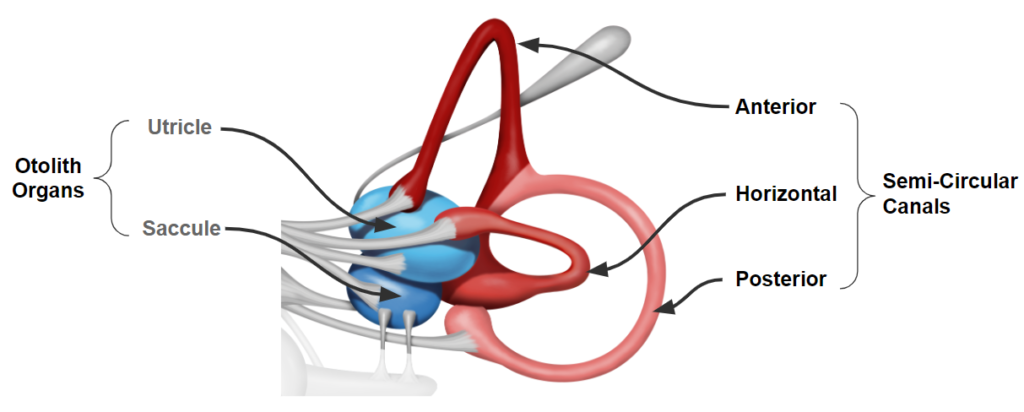
Caption: The three canals of the peripheral vestibular system
The patient’s eyes demonstrate a brisk left horizontal beat (toward the ground) while the patient yells out “I’m spinning!” when the patient’s head is turned left, so you reassure the patient and watch as the nystagmus settles out after about 15 seconds. After putting the patient’s head back to center, you move it to the right. There you observe a right horizontal beat nystagmus (again, toward the ground) lasting about 10 seconds, which is less intense (and the patient says, “I still feel it, but that’s not so bad”). Just to fully reassure yourself that the nystagmus is likely due to a peripheral issue and not a stroke, you put on the visual fixation lights on your infrared video goggles during a re-test of the supine roll test, and as you hoped, the nystagmus diminishes in intensity as soon as the fixation lights are turned on. This finding is consistent with a peripheral vestibular condition, rather than a central vestibular issue such as stroke. You’re on the right track now!

Caption: Right horizontal beat nystagmus seen in infrared video goggles in a right head turn position during the supine roll test
What’s your diagnosis? For most vestibular clinicians, the answer would be a left horizontal canalithiasis BPPV, since the nystagmus beats toward the ground on both sides of the supine roll test, and in that case, the side with more intense symptoms is usually the affected side. There are many options to treat this, but you choose to go with a gentle and traditional BBQ roll (also known as the Lempert or log roll).
As you patiently and methodically roll the patient toward their right side, onto their stomach, and then back to upright, taking at least 30 seconds in each position, you find that the patient, although “woozy,” doesn’t have that spinning sensation any more. Upon a final re-test of the supine roll test, they have no nystagmus and no more vertigo! It’s time to send this patient home with education on reducing risk factors for recurrent BPPV (keep their hypertension well-managed and vitamin D levels at a healthy level. You give them information on how to follow-up with an outpatient vestibular physical therapist. As they head out, the patient says, “You’re my HERO.” And today, you really are glad you learned how to be a dizziness detective for patients in the ED!
Does this case resonate with any of your experiences? Have you ever wanted to learn more about how to help patients with dizziness in the ED? The EXCITING news is that we have more top-notch vestibular content coming, tailored to clinicians working in the ED and acute care hospital settings. Keep an eye out for podcasts, a webinar, and an in-person course ahead, so you can enhance your role as a heroic dizziness detective!
References
- Kattah JC. Update on HINTS Plus, With Discussion of Pitfalls and Pearls. J Neurol Phys Ther. 2019 Apr;43 Suppl 2:S42-S45.
- Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov;40(11):3504-10.
- Kim CH, Jeong H, Shin JE. Incidence of idiopathic benign paroxysmal positional vertigo subtype by hospital visit type: experience of a single tertiary referral centre. J Laryngol Otol. 2023 Jan;137(1):57-60.
- Newman-Toker DE, Kerber KA, Hsieh YH, Pula JH, Omron R, Saber Tehrani AS, Mantokoudis G, Hanley DF, Zee DS, Kattah JC. HINTS outperforms ABCD2 to screen for stroke in acute continuous vertigo and dizziness. Acad Emerg Med. 2013 Oct;20(10):986-96.
- Tarnutzer AA, Berkowitz AL, Robinson KA, Hsieh YH, Newman-Toker DE. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. CMAJ. 2011 Jun 14;183(9):E571-92.
- van Dam VS, Maas BDPJ, Schermer TR, van Benthem PG, Bruintjes TD. Two Symptoms Strongly Suggest Benign Paroxysmal Positional Vertigo in a Dizzy Patient. Front Neurol. 2021 Jan 14;11:625776.a

Great article!!
Thank you Stefanie!