DizzyDx™ can help Physical Therapists be primary care game-changers for patients who visit the ED with ANS and immune reactivity.
Assistant Professor, South College Atlanta
CEO and Co-Founder DizzyDx.com
What is DizzyDx™?
DizzyDx™ is a clinical decision support tool to help physical therapists evaluate dizziness. It is an innovative web-based application that can be used on any device with internet access. DizzyDx™ offers a decision tree algorithm to consider symptoms discussed in the patient interview alongside common clinical patterns in which symptoms commonly occur. Hypothesized impairments are presented as a clinician considers a clinical case of interest and is encouraged to perform and interpret clinical testing to rule in/out impairments to progressively refine a differential diagnosis. DizzyDX™ cites >200 references that are consistently updated for further review of current best practice.
How can a clinical decision support tool help a physical therapist in the ED?
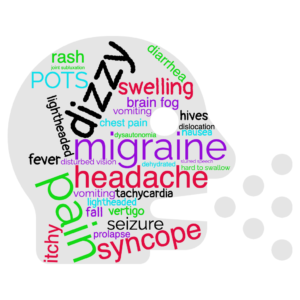
Dizziness alone is not likely a symptom worthy of a visit to the ED. Dizziness can be a sign of an acute stroke and is a poor prognostic indicator following head trauma. Acute dizziness accompanied with nausea and vomiting may result in dehydration and might require differentiation between BPPV, acute labyrinthitis or migraine activity. Dizziness can also present as a side effect to several medications and can be associated with syncope, falls, and further injury that may result in a visit to the ED.
Physical therapists can assist with the triage process by effectively interviewing patients, the symptom presentations, risk factors and possible impairments contributing to dizziness and impaired functional abilities. While medical providers may assess for life threatening disease processes, physical therapists are equipped to evaluate threats to safety and may help provide much needed patient education, support, advocacy, and resource dissemination alongside the successful identification of referrals, need for ED observation, or inpatient admission. DizzyDx™ is a subscription-based resource for individual professional development, to facilitate mentoring staff, students, and residents, and to build consistency in care offered by departments and across teams.
What are Dysautonomia and POTS and why do they occur?
Dysautonomia is a broad term used to describe an acute, subacute, or chronic state in which homeostasis is disrupted. The regulation of autonomic nervous system body functions, such as heart rate and blood pressure responses to changes in position or activity level, digestion, regulation of body temperature, pupillary responses, and bowel and bladder activity may cause symptoms and/or interfere with routine daily activities.
Dysautonomia may be triggered by an event such as a viral infection, surgical procedure, exposure to anesthesia, traumatic accident (particularly that results in head trauma or concussion), an allergic or immune response, or stress., Dysautonomia can also be associated with other cardiovascular, pulmonary, endocrine, and neurological disorders. Dysautonomia may be transient and may resolve over time or it may evolve into a chronic state that requires a multidisciplinary approach to care.
Orthostatic Hypotension (OH) is a form of dysautonomia associated with a blood pressure drop when changing body positions, most often associated with venous pooling. Individuals with OH may present to the ED with an injury due to associated syncope and falls. Individuals with progressive neurological disorders such as Parkinson’s disease, Lewey body dementia, multiple systems atrophy or pure autonomic failure may experience progressive difficulty with OH. Those with diabetes may find OH to be indicative of poor glucose regulation. The otolith organs are involved in blood pressure regulation through a vestibular sympathetic reflex that is coupled with the baroreflex and cerebral perfusion.
Postural Orthostatic Tachycardia Syndrome (POTS) is another type of dysautonomia that has diagnostic criteria and can be easily screened in the ED. POTS is characterized by a chronic and marked increase in pulse rate when moving from supine to standing. The Active Stand Test (aka, Poor Man’s Tilt Test, in the absence of instrumented Tilt Table Test) requires a 10 minutes of quiet supine rest followed by 10 minutes of quiet standing. In some instances, a NASA Lean Test may be conducted where the individual stands up against the wall to minimize activation of active muscle pumping in the legs.
| Active Stand Test Tilt Table Test | Fall in Systolic BP upon standing | Fall in Diastolic BP upon standing | Increase in HR upon standing | Timing |
| Classic OH | >20 mmHg | >10 mmHg | Not specified | Sustained BP fall within 3 min. of standing |
| POTS | SBP fall not meeting OH criteria | DBP fall not meeting OH criteria | >30 bpm or >120Ages 12-19:>40 bpm or >120 | Sustained HR increased within 10 minutes of standing |
| Vasovagal Syncope | No formal pattern due to heterogenous hemodynamic patterns. HR slowing may or may not be present. If syncope is symptomatic with drop in BP, OH is likely the cause. If syncope is asymptomatic with drop in BP, OH may be the cause. | |||
Active Stand Test and Interpretation
Thijs RD, Brignole M, Falup-Pecurariu C, et al. Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness: Consensus statement of the European Federation of Autonomic Societies (EFAS) endorsed by the American Autonomic Society (AAS) and the European Academy of Neurology (EAN). Clin Auton Res. 2021;31(3):369-384. doi:10.1007/s10286-020-00738-6.
Why do people with Dysautonomia and POTS seek care in the ED?
Syncope can be a primary problem for individuals with dysautonomia. An individual may seek urgent/emergent care if syncope is recurrent or if there is evidence of head trauma after a syncope episode and a fall. Additionally, some individuals may have seizure-like activity coupled with syncope.
Current research related to immune susceptibility indicates that some individuals may exhibit relapsing and remitting episodes or dysautonomia conditions with acute on chronic presentations that may represent a ‘crisis’ or need for emergency care/support.
What can be offered to people with Dysautonomia and POTS in the ED?
As Dr. Rebekah Griffith indicates, safety is a primary concern addressed by physical therapists for those who visit the ED. Safety related to dysautonomia is most directly related to fall risk and syncopal episodes. A neuro screen and detailed history related to functional status and the home environment may be critical to determining patient safety. Recognition of joint hypermobility can be very important as joint dislocations/subluxations and chronic pain may be a comorbid factor in many cases and the overlap of symptoms may lead a person to an acute state requiring medical attention.
An alternative concern related to safety involves self-care and coping through a health crisis. People across the spectrum of excellent to poor health literacy, support networks, and access to healthcare resources may experience health crises that require evaluation and guidance of a compassionate provider. Active listening and validation of one’s perceived traumatic situation go a long way to helping diffuse a situation that may be escalating with threats to a person’s safety and security.
Active listening and validation of symptoms coupled with patient education to help discover a trigger for the presenting flare can help de-escalate anxiety and loss of self-regulation. Autonomic neuropathy can be associated with dysautonomia, and use of the COMPASS-31 can help identify clusters of symptoms to help target effective referrals and patient education in the ED. Supplemental materials are available online for the COMPASS-31 tool and scoring using the Treister R, et al. validation study.
Some dysautonomia flares respond to hydration or volume expansion. Rate of IV infusion in the ED can be important to avoid “3rd spacing” (movement of fluid from vasculature into interstitial space) for someone who is already experiencing pooling of blood in the legs and abdominal bloating. A study looking at the effects of IV hydration versus
What is Mast Cell Activation Syndrome (MCAS) and why do people experience it?
Mast cells are part of our normal immune response to allergens. Mast Cell Activation occurs when the body reacts to an exposure to a chemical, food, infection, or other source. Mast Cell Activation Syndrome (MCAS) represents an IgE hypersensitivity reaction where the mast cells degranulate or proliferate in an unregulated manner, which can result in a prolonged lower threshold response to an antigen. Mast cells are found in every tissue of the human body, including within the brain and therefore mast cell degranulation has many varied presentations. There are a number of mediators involved in the immune response and you can learn more with the Mast Cell Primer.
Why might someone seek help in the ED for an MCAS flare?
Mast cell activation has very poor diagnostic testing available. Serum tryptase and 24-hour urine testing must be initiated within 2 hours of mast cell activation and most people don’t know when the trigger starts or that regranulation has even occurred. The clinical diagnosis is based on chronic aberrant mast cell activation in at least 2 organ systems. It is estimated that at least 17% of the population is affected by MCAS.
How can a physical therapist engage with a person who has MCAS?
A person who arrives to the ED may not be aware of MCAS as a confounding factor impacting a flare of symptoms. A review of systems including a scratch test for dermatographia, and a thorough history to investigate signs of early anaphylaxis are helpful to promoting awareness of immune reactivity that may be unrecognized by the patient or their current providers.
For people engaged in physical therapy, signs of MCAS can be an immediate or delayed response to exercise/activity.,, Discuss antihistamine management of identified signs of mast cell activation with the medical team and facilitate documentation to the primary or specialty providers as well as tertiary providers such as physical therapists to help educate team members about mast cell involvement in acute dysautonomia flares. As an ED Team, provide materials to recommend over the counter antihistamine trials until a person can achieve access to a provider who is experience with MCAS management can offer comprehensive care.
THE WHY? Empower PTs to make the ED experience better for people with invisible acute crises. People need support when they are in crisis and are often dismissed as having a mental health issue with a psych consult in the ED due to poor coping skills and self regulation. It has been reported by the Vestibular Disorders Association (VeDA) that people with complex and chronic health conditions such as the ones discussed see > 5-7 MDs before acquiring a diagnosis. Specialty provider appointments often have prolonged waiting lists and physical therapists can be instrumental in partnering with patients to identify symptom triggers and to address specific impairments to help turn down the volume of ANS and immune reactivity until medical help can be acquired. PTs are primary care providers and need innovative tools like DizzyDx™ to help with clinical reasoning.
DizzyDx™ helps physical therapists recognize symptoms and impairments that interfere with daily activity. It IS all in the head with convergence and overlap of neuroanatomical pathways. Investigate the autonomic nervous system (ANS) and immune system contributions to dizziness. It is never too late to learn new ways to help people and to embrace advances in our understanding of human functioning.
References:
1 Raj SR, Arnold AC, Barboi A, et al. Long-COVID postural tachycardia syndrome: an American
Autonomic Society statement. Clin Auton Res. 2021;31(3):365-368. doi:10.1007/s10286-021-00798-2
2 Forstenpointner J, Elman I, Freeman R, Borsook D. The omnipresence of autonomic modulation in
health and disease. Prog Neurobiol. 2022;210:102218. doi:10.1016/j.pneurobio.2022.102218
3 Freeman R, Abuzinadah AR, Gibbons C, Jones P, Miglis MG, Sinn DI. Orthostatic Hypotension: JACC
State-of-the-Art Review. J Am Coll Cardiol. 2018;72(11):1294-1309. doi:10.1016/j.jacc.2018.05.079
4 Bogle JM, Benarroch E, Sandroni P. Vestibular-autonomic interactions: beyond orthostatic
dizziness. Curr Opin Neurol. 2022;35(1):126-134. doi:10.1097/WCO.0000000000001013
5 Wang E, Ganti T, Vaou E, Hohler A. The relationship between mast cell activation syndrome, postural
tachycardia syndrome, and Ehlers-Danlos syndrome. Allergy Asthma Proc. 2021;42(3):243-246.
doi:10.2500/aap.2021.42.210022
6 Treister R, O’Neil K, Downs HM, Oaklander AL. Validation of the composite autonomic symptom scale
31 (COMPASS-31) in patients with and without small fiber polyneuropathy. Eur J Neurol.
2015;22(7):1124-1130. doi:10.1111/ene.12717
7 Blitshteyn S, Doherty TA. Intravenous saline may not be a placebo in patients with small fiber
neuropathy. Muscle Nerve. 2023;67(6):E25-E26. doi:10.1002/mus.27826
8 Slee VM, et al. What are Mast Cell Diseases in The Mast Cell Disease Primer, The Mast Cell Disease
Society website, available at https://tmsforacure.org/what-are-mast-cell-diseases/#mast-cell-activation-
syndromes. Published 2021. Accessed 3/01/2024.
9 Afrin LB, Ackerley MB, Bluestein LS, et al. Diagnosis of mast cell activation syndrome: a global
“consensus-2”. Diagnosis (Berl). 2020;8(2):137-152. Published 2020 Apr 22. doi:10.1515/dx-2020-0005
10 Cardona V, Ansotegui IJ, Ebisawa M, et al. World allergy organization anaphylaxis guidance
2020. World Allergy Organ J. 2020;13(10):100472. Published 2020 Oct 30.
doi:10.1016/j.waojou.2020.100472
11 Giannetti MP. Exercise-Induced Anaphylaxis: Literature Review and Recent Updates. Curr Allergy
Asthma Rep. 2018;18(12):72. Published 2018 Oct 26. doi:10.1007/s11882-018-0830-6
12 Kulinski JM, Metcalfe DD, Young ML, et al. Elevation in histamine and tryptase following exercise in
patients with mastocytosis. J Allergy Clin Immunol Pract. 2019;7(4):1310-1313.e2.
doi:10.1016/j.jaip.2018.07.008
13 Romero SA, McCord JL, Ely MR, et al. Mast cell degranulation and de novo histamine formation
contribute to sustained postexercise vasodilation in humans. J Appl Physiol (1985). 2017;122(3):603-610.
doi:10.1152/japplphysiol.00633.2016
Additional Resources:
-
- Dysautonomia International: http://www.dysautonomiainternational.org/
-
- Dysautonomia International Webinar Library: https://vimeo.com/dysautonomia
-
- ME Action – UK – US – Research: https://www.meaction.net/news/research/
-
- NeuroImmune Foundation: https://neuroimmune.org/
-
- Open Medicine Foundation: https://www.omf.ngo/the-end-mecfs-project/
-
- Primary Immunodeficiency Foundation: https://primaryimmune.org/
-
- The Ehlers Danlos Society: https://www.ehlers-danlos.com/what-is-eds/
-
- The Mastocytosis Society: https://tmsforacure.org/
-
- Workwell Foundation: https://workwellfoundation.org/

Thank you, Rebekah!